Improving patient outcomes with artificial intelligence, machine learning, and wearable devices
The primary goal of our lab is to develop computational analyses and tools that reach patient care to improve outcomes. The convergence of machine learning and expansive routine clinical data enable the development of automated predictive models. However, many barriers remain, impacting the real-world accuracy, deployability, and clinical benefit of artificial intelligence and predictive tools.
One of our priorities is to manage and reduce toxicity of cancer therapy. We developed an electronic health record-based machine learning algorithm to predict acute care visits during outpatient cancer therapy (Hong, JCO Clin Cancer Inform 2018). This model was evaluated in one of the first prospective randomized studies of clinical machine learning, demonstrating that its use directed clincial management to reduce rates of acute care during cancer therapy (Hong, J Clin Oncol 2020).
This experience has enabled early novel studies evaluating a number of important considerations in the implementation of artificial intelligence in clinical practice, including cost reductions (Natesan, NEJM AI 2024), implementation (Hong, BMC Bioinformatics 2022) and healthcare provider reception (Hong, BMJ Health Care Inform 2023). We have since expanded this work into wearable devices, leading one of the first studies developing a wearable-based machine learning model to predict adverse events built off of three prospective trials (Friesner, JAMA Oncol), which is planned for validation on a national clinical trial, NRGF-001.

Personalizing treatment and accelerating clinical trials in prostate cancer
Prostate cancer is the second most common cause of cancer death among men in the United States. Advances in medical imaging, particularly in prostate specific membrane antigen positron emission tomography (PSMA PET) have led to earlier detection of a subtype of metastatic prostate cancer called oligometastatic prostate cancer, where the cancer has spread to only a few other areas of the body. These patients have a better chance at survival, and radiation treatments to the prostate and areas of metastatic cancer have been found to improve long-term outcomes and offer a potential cure.
Our team has specific clinical expertise in the treatment of prostate cancer, which we are combining with our expertise in artificial intelligence. We developed evidence from early seminal trials showing that patients with prostate oligometastasis are most likely to have long-term disease control with targeted radiation to metastases (Hong, PLOS ONE 2018). We are now applying computer vision approaches to PSMA PET to 1) identify how stage migration has impacted best candidates for prostate radiation, which has been shown to improve survival in metastatic prostate cancer and 2) identify patients who benefit most from targeted radiation to metastasis (Chen, ASTRO 2023).
Clinical trials in prostate cancer also require extended follow-up to report results, which limits the rate of delivering advances to patients. Our team is applying machine learning approaches to a large portfolio of phase III clincial trials to develop methods to expedite reporting and accelerate the pace of progress.
Among other studies, our team has also developed a tool to estimate testosterone recovery following androgen deprivation (Spiegel, Int J Radiat Oncol Biol Phys 2019).


Natural language processing and unlocking unstructured clinical data
Large amounts of data are captured in free-text clinical notes, which can pose challenges to clinical study. Extracting this unstructured information can both inform clinical research and facilitate deployable computational tools. The emergence of generative artificial intelligence approaches to natural language processing also carries significant promise in both research and clinical practice (Waters, Pract Radiat Oncol 2023).
We conducted early studies to compare the ability of natural language processing to extract patient outcomes during cancer therapy from routine clinical documentation versus physicians. Our studies indicate high variability even among clinician experts, which may motivate the use of computational approaches (Fairchild, Int J Radiat Oncol Biol Phys 2020). Our natural language processing pipeline facilitates systematic extraction of patient symptoms during cancer therapy (Hong, JAMIA Open 2020).

Learning from real world data
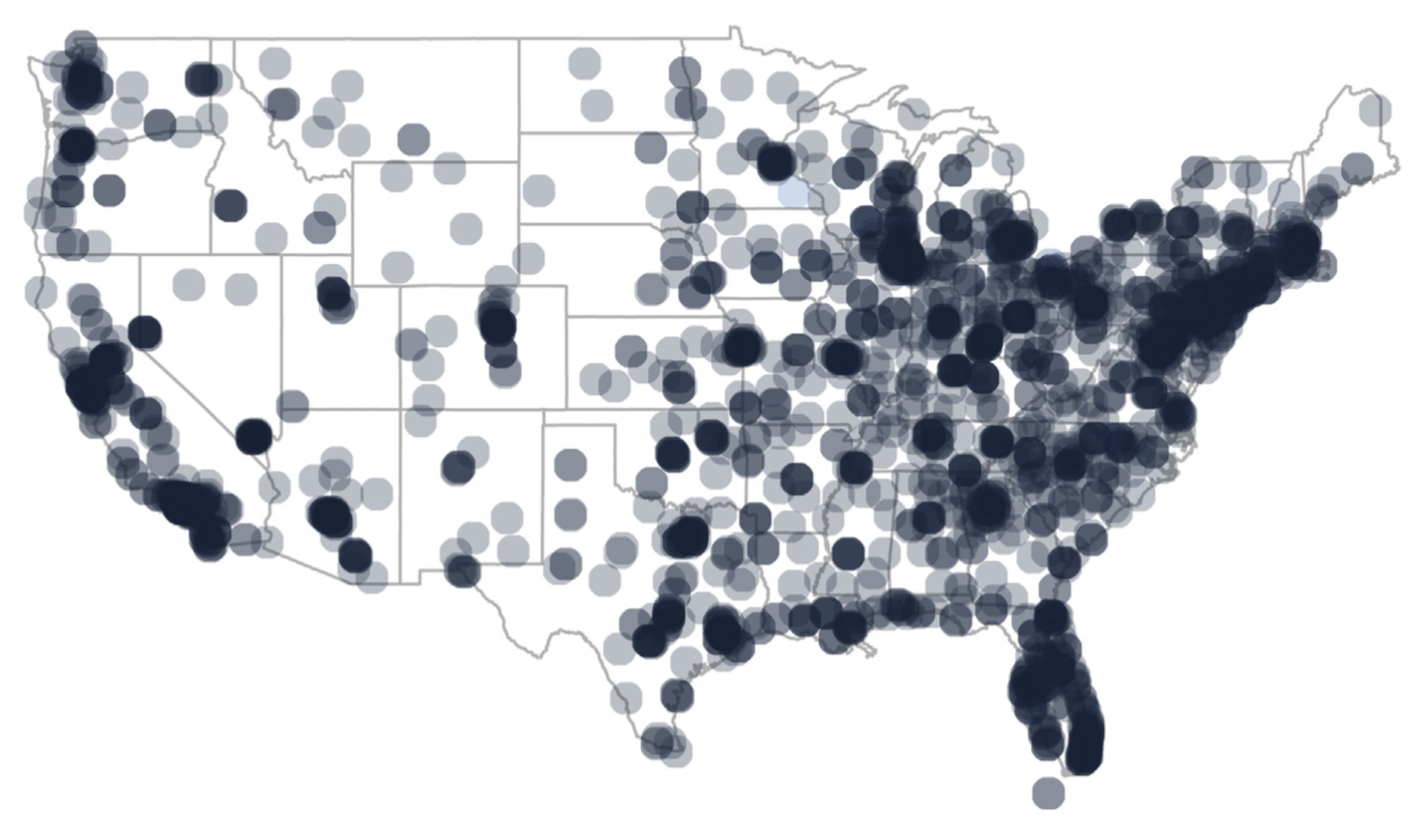
Real world data offers insights that can complement randomized controlled clinical trials. This can provide information regarding practice patterns and generate knowledge to inform future trials. Our team has expertise analyzing data from electronic health records, national databases, institutional experiences, claims data, and payor data to both learn from prior experiences and characterize data limitations (Hong, JAMA Netw Open 2021).
A priority of our work also focuses on physician and patient interactions with electronic health records and health information technology (Huilgol, Cancer Med 2022). Among these studies, we have disparities in patient enrollment to online patient portals (Sinha, JAMA Oncology 2021) and characterized electronic health record use of oncologists compared to other physician specialties (Sinha, JNCI Cancer Spectr 2023).
We have also evaluated practice patterns in a range of cancers including lung (Hong, J Natl Compr Canc Netw 2019), prostate, and gynecologic malignancies. Among these studies, we have used Medicare provider data to identify disparities in access to specialized therapies for prostate and gynecologic malignancies (Hong, Brachytherapy 2018).