Pioneering clinical studies of medical artificial intelligence
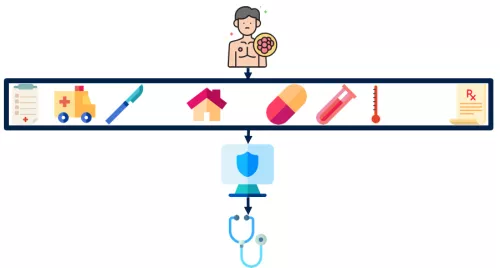
Our team has led early end-to-end efforts to develop and implement healthcare AI to improve outcomes for patients.
Firsts in clinical AI
We developed an electronic health record-based machine learning algorithm to predict acute care visits during outpatient cancer therapy (Hong, JCO Clin Cancer Inform 2018). This model was evaluated in one of the first prospective randomized studies of clinical machine learning, demonstrating that its use directed clinical management to reduce rates of major adverse events resulting in emergency visits and hospitalizations during cancer therapy (Hong, J Clin Oncol 2020), also leading to practical reductions in healthcare costs (Natesan, NEJM AI 2024).
Understanding implementation
Integrating AI into clinical workflows remains a challenge. Our end-to-end experience has enabled unique insights into overcoming barriers to implementation (Hong, BMC Bioinformatics 2022) and healthcare team reception (Hong, BMJ Health Care Inform 2023).
Leading national efforts
We lead an NIH/NCI-funded effort across multiple institutions ranging from academic practices to community practices to expand the reach of our AI algorithms.
Integrating wearable devices and novel data sources to improve care
Our team is committed to expanding useful data collected in clinical care. Among these is our expertise in patient-generated health data, particularly in wearable devices and patient-reported outcomes (PROs) to better capture health status and quality of life.
We have developed pioneering algorithms across novel data domains, particularly in patient-generated health data with wearable devices. Our team leveraged wearable device data in early clinical trials of patient activity monitoring to build machine learning models to enable early identification of patients who require additional clinical support (Friesner, JAMA Oncol 2024). These algorithms are now being tested in the clinic on the Wearable Activity Tracking to Curb Hospitalizations (WATCH) Trial and the national clinical trial NRGF-001.
Personalizing treatment and accelerating clinical trials in prostate cancer
Our team has specific clinical expertise in prostate cancer, enabling specific advances in treating the second most common cause of cancer death among men in the United States.
We are supported by a Prostate Cancer Foundation Challenge Award to accelerate clinical trials in prostate cancer, which typically require years to decades to bring new treatments to patients.
We have developed AI-based approaches to predict the outcomes of clinical trials based on routine data acquired during the first few months of a new treatment. These approaches have been tested and validated on large, practice-changing trials in prostate cancer. (Sabbagh, ASCO 2024).

Multi-modal data integration is a fundamental component of medical AI. Our team is integrating all elements of a patient's journey to improve clinical decision making. Among these is our clinical expertise in oligometastatic prostate cancer and the utilization of PSMA PET, which we are studying to better identify treatments (Chen, JNCI Spectrum 2025). We are expanding this work to integrate our ongoing efforts in digital pathology and biomarkers to create fully multi-modal representations of cancer.

Natural language processing and large language models to unlock clinical data
Our team has extended experience in applying natural language processing to empower cancer care.
Large amounts of data are captured in free-text clinical notes, which can pose challenges in usability. Our team both advances natural language processing (NLP) and large language model (LLM) approaches and applies these methods.
We conducted early studies demonstrating the variability of physician experts in retrieving information from clinical text (Fairchild, Int J Radiat Oncol Biol Phys 2020), developing a natural language processing pipeline facilitates systematic extraction of patient symptoms during cancer therapy (Hong, JAMIA Open 2020).
With the emergence of large language models and generative AI, we have pioneered work in adapting them for clinical use and for applying them to clinical problems, including inference from radiology reports (Chen, JCO Clin Cancer Inform 2024) and evaluating patient portal messages (Chang, JCO Clin Cancer Inform 2025). These efforts set the stage for automated efforts to improve clinical triage.
Our work also includes developing methodological recommendations for adapting language models to clinical applications (Chen, ML4H, 2025).

Learning from real world data
Real world data offers insights that can complement randomized controlled clinical trials. This can provide information regarding practice patterns and generate knowledge to inform future trials. Our team has expertise analyzing data from electronic health records, national databases, institutional experiences, claims data, and payor data to both learn from prior experiences and characterize data limitations (Hong, JAMA Netw Open 2021).
A priority of our work also focuses on physician and patient interactions with electronic health records and health information technology (Huilgol, Cancer Med 2022). Among these studies, we have disparities in patient enrollment to online patient portals (Sinha, JAMA Oncology 2021) and characterized electronic health record use of oncologists compared to other physician specialties (Sinha, JNCI Cancer Spectr 2023).
We have also evaluated practice patterns in a range of cancers including lung (Hong, J Natl Compr Canc Netw 2019), prostate, and gynecologic malignancies. Among these studies, we have used Medicare provider data to identify disparities in access to specialized therapies for prostate and gynecologic malignancies (Hong, Brachytherapy 2018).